Cough and cold
Coughs and colds are extremely common in young children. Over the first few years of life, your child might have these every month.
-
Coughing is the body's natural way of clearing infection
-
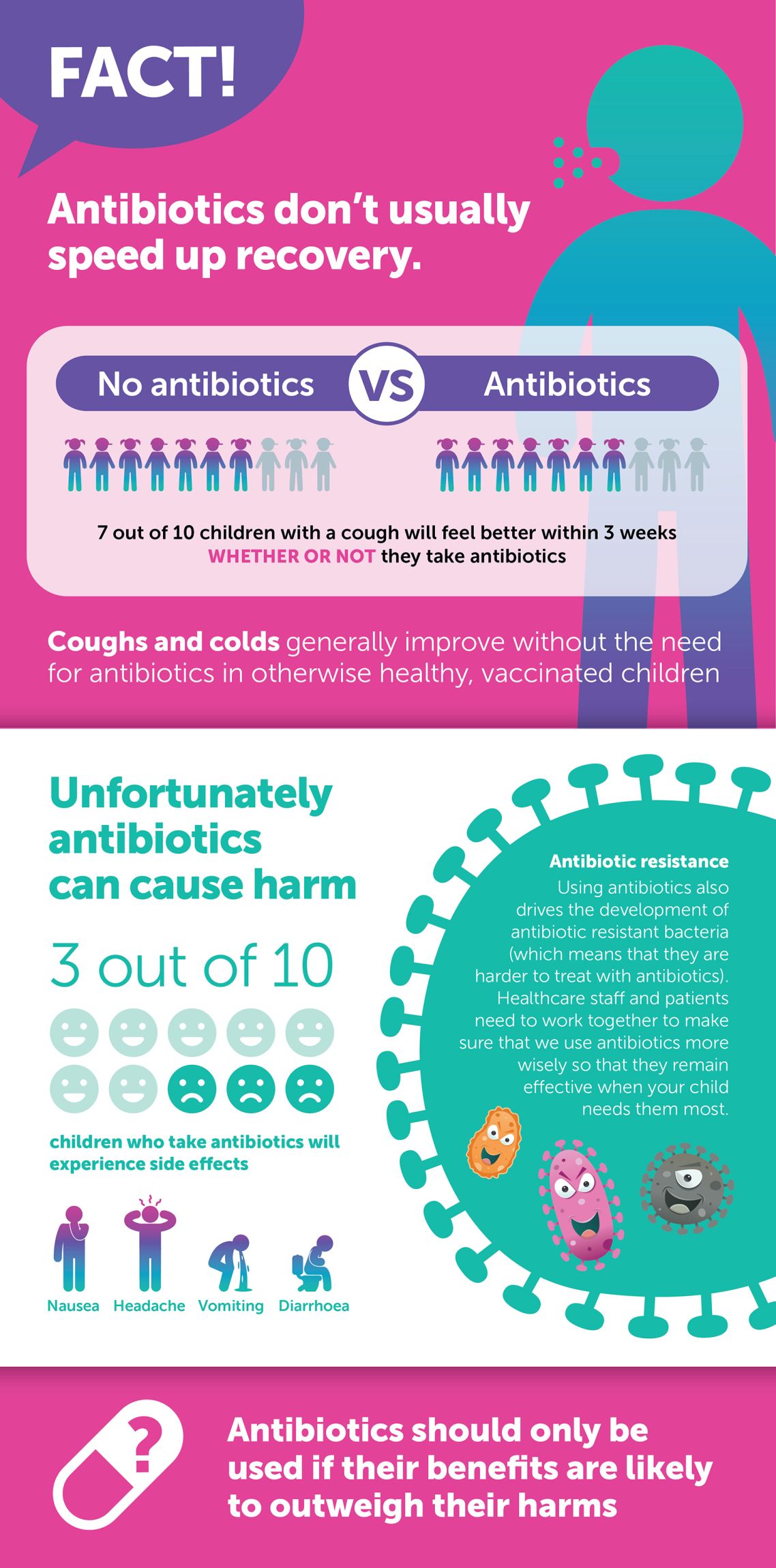
Most of these are likely to be caused by a virus, which means that antibiotics don’t help. Antibiotics might cause side effects such as rash and diarrhoea, or increase the risk of developing antibiotic resistance
-
Having green snot or a noisy chest does not mean that your child has an infection needing antibiotics
-
Coughing can wake a child in the night but does not mean the illness is more severe
Related topics: asthma, bronchiolitis, Covid-19, croup, difficulty breathing
When should you worry?
If your child has any of the following:
- Breathing very fast or breathing that stops or pauses
- Making a grunting noise every time they breathe out
- A harsh breath noise as they breathe in (stridor) present all of the time (even when they are not upset)
-
Becomes pale, blue, mottled and or unusually cold to touch
-
Difficult to wake up, very sleepy or confused
-
Weak, high-pitched, continuous cry or can’t be settled
-
Has a fit (seizure)
-
Is under 3 months old with temperature more than 38°C or under 36°C (unless fever in the 48 hours following vaccinations and no other red or amber features)
-
Has a rash that does not go away with pressure (the ‘Glass Test’)
You need urgent help
Go to the nearest Hospital Emergency (A&E) Department or phone 999
If your child has any of the following:
- Working hard to breathe, drawing in of the muscles below the ribs
- A harsh breath noise as they breathe in (stridor) only when upset
-
Dry skin, lips or tongue
-
Not had a wee or wet nappy in last 8 hours
-
Poor feeding in babies (less than half of their usual amount)
-
Irritable (Unable to settle them with toys, TV, food or hugs even after their fever has come down)
-
Is 3-6 months old with temperature 39°C or above (unless fever in the 48 hours following vaccinations and no other red or amber features)
-
Temperature of 38°C or above for more than 5 days or shivering with fever(rigors)
-
Temperature less than 36°C in those over 3 months
-
Getting worse or you are worried about them
You need to contact a doctor or nurse today
Please call your GP surgery or contact NHS 111 - Go to 111.nhs.uk or call 111.(111 online does not currently take questions about children aged under 5, so if your child is 4 or younger, please call 111).
If symptoms persist for 4 hours or more and you have not been able to speak to either a member of staff from your GP practice or to NHS 111 staff, recheck that your child has not developed any red features.
If none of the above features are present
-
Watch them closely for any change and look out for any red or amber symptoms
-
Additional advice is also available for families for help cope with crying in otherwise well babies
-
If your child has a long term condition or disability and you are worried please contact your regular team or follow any plans that they have given you.
Self care
Continue providing your child’s care at home. If you are still concerned about your child, call NHS 111 – dial 111
What should you do?
-
Keep your child well hydrated by offering them lots to drink
-
Most children with coughs and colds do not require treatment with antibiotics
-
If your child seems to be in pain or discomfort, you can give your child paracetamol or ibuprofen, following the instructions on the container
-
Do not give cough syrup. It is not recommended for children under 6 years. It can make children sleepy and does not help
-
Try using saline nose drops or spray if your baby has a blocked nose
-
For children over 1 year, a spoon of honey (perhaps in a warm drink) half an hour before bed may help them to wake less often in the night
-
For children over 2 years, vapour rubs (containing camphor, menthol and/or eucalyptus) may help children sleep better
How long will your child's symptoms last?
-
Coughs and colds can continue for weeks before they get better
-
Over the winter, children are likely to get one viral infection after another, which can make you think that they are never well. Things will get better in the summer months
-
Having a cough for 2 or 3 weeks does not mean that your child needs antibiotics
-
Children under 2 years of age with breathing difficulty may have bronchiolitis. This is a common condition that usually starts as a runny nose and cough, but their breathing may get worse over the next 2-3 days
-
If your child has noisy breathing, they might have croup

The diagrams above are taken from www.whenshouldiworry.com
Where should you seek help?
- If it is non-urgent, speak to your local pharmacist or health visitor
- If your child has any of the above features, urgently see your GP. For an urgent out-of-hours GP appointment, call NHS 111
- You should only call 999 or go to your nearest Emergency Department (A&E) in critical or life threatening situations
For wear and tear, minor trips and everything in between
Self-care
You can treat your child's very minor illnesses and injuries at home.
Some illnesses can be treated in your own home with support and advice from the services listed when required, using the recommended medicines and getting plenty of rest.
Sound advice
Children can recover from illness quickly but also can become more poorly quickly; it is important to seek further advice if a child's condition gets worse.
For information on common childhood illnesses go to What is wrong with my child?
Pharmacists are experts in many aspects of healthcare and can offer advice on a wide range of long-term conditions and common illnesses such as coughs, colds and stomach upsets. You don’t need an appointment and many have private consultation areas, so they are a good first port of call. Your pharmacist will say if you need further medical attention.
Sound advice
- Visit a pharmacy if your child is ill, but does not need to see a GP
- Remember that if your child's condition gets worse, you should seek further medical advice immediately
- Help your child to understand - watch this video with them about going to the pharmacy
For information on common childhood illnesses go to What is wrong with my child?
The 0-19 Service for children and young people is delivered by Oxford Health NHS Foundation Trust and offers a single point of access for Health Visiting, School Nursing and the Family Nurse Partnership. You can contact the teams using the details below:
Single Point of Access (SPA): 01865 903 800
Email: cyp0-19@oxfordhealth.nhs.uk
Chat Health Parentline
Text us any time for confidential advice and support and you will have a response the next working day (Monday-Friday exluding Bank Holidays).
Parents and carers for children aged 0-4: Text 07312 263 081
Parents and carers of children aged 5-11: Text 07312 263 227
Young people aged 11-19 and their parents and carers: Text 07312 263 08
Health Visitors
Health visitors are registered nurses or midwives who have additional training in community public health nursing. They provide a universal service, targeted to individual needs for children aged 0-5 years. Learn more about the Oxfordshire Health Visiting Service here!
School and college Health Nurses
School Health Nurses are specialist public health nurses and have offices across Oxfordshire. They work very closely with Health Visitors to support school aged children. They are available for young people to access in secondary schools and colleges, and offer a service to children who are home educated. They work closely with children, young people and their families to support and promote health and wellbeing. Learn more about the Oxfordshire School and college Health Nursing Service here!
Family Nurse Partnership
The Family Nurse Partnership service supports parents who are aged 19 years or under at conception, or under 21 years if they have been in care. The Family Nurse works alongside younger parents in their home, offering health, wellbeing and development support and information from the early stages of pregnancy, usually up until your child is two. Learn more about the Family Nurse Partnership service here!
GPs assess, treat and manage a whole range of health problems. They also provide health education, give vaccinations and carry out simple surgical procedures. Your GP will arrange a referral to a hospital specialist should you need it.
Sound advice
You have a choice of service:
- Doctors or GPs can treat many illnesses that do not warrant a visit to A&E
- Help your child to understand – watch this video with them about visiting the GP or going to a walk in centre
For information on common childhood illnesses go to What is wrong with my child?
If you’re not sure which NHS service you need, you can call 111 or use 111 online.
Please note that 111 online is for people aged 5 and over. Call 111 if you need help for a child under 5.
An adviser will ask you questions to assess your symptoms and then give you the advice you need, or direct you straightaway to the best service for you in your area.
Sound advice
Use NHS 111 if you are unsure what to do next, have any questions about a condition or treatment or require information about local health services
For information on common childhood illnesses go to What is wrong with my child?
Emergency Departments (A&E) provide vital care for life-threatening emergencies, such as loss of consciousness, suspected heart attacks, breathing difficulties, or severe bleeding that cannot be stopped. If you’re not sure it’s an emergency, call 111 for advice.





